Learn about the PA profession in Canada
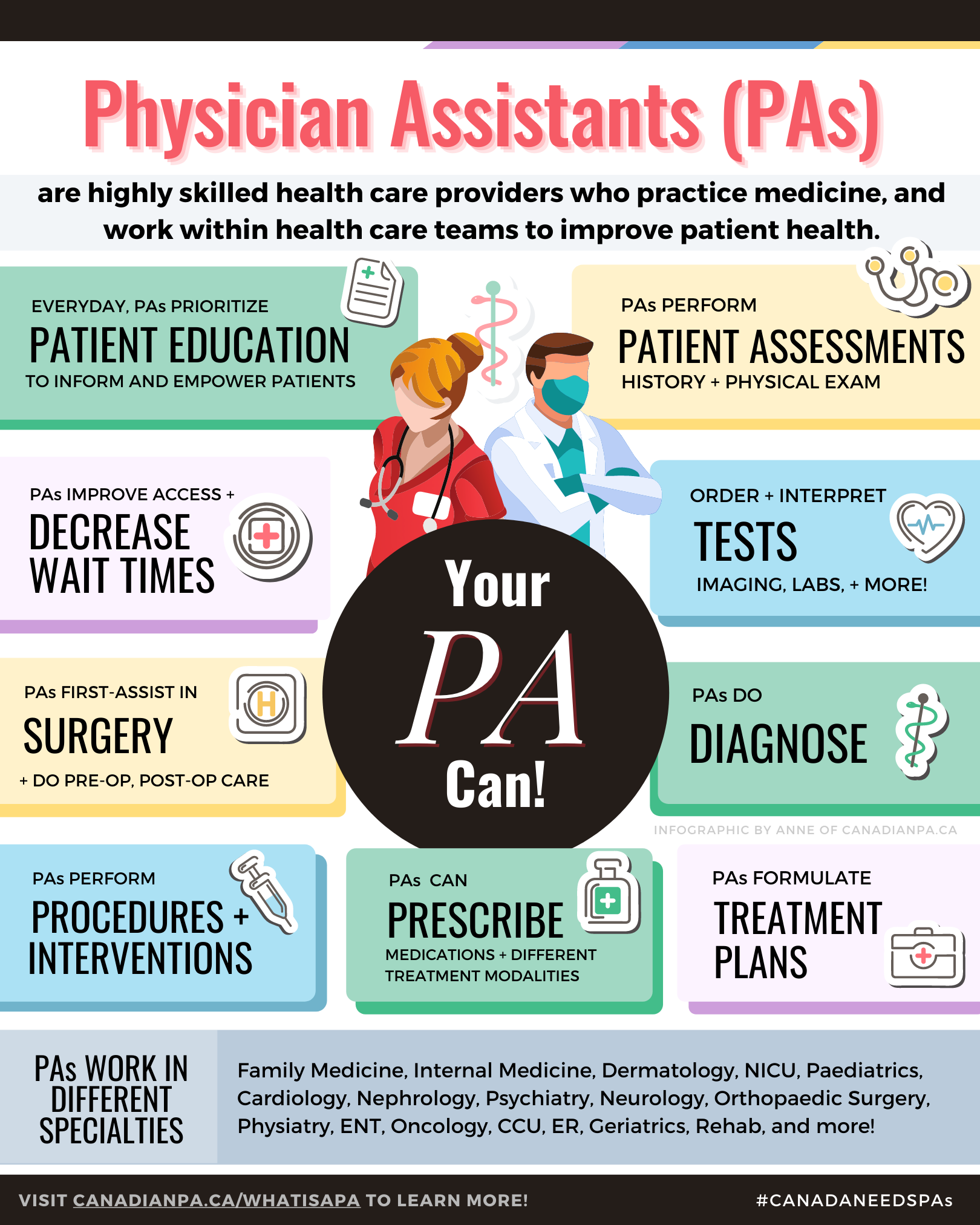
The role of Physician Assistants has emerged as a vital component of the healthcare workforce in Canada.
These highly skilled professionals play a crucial role in bridging the gap between physicians and patients, thereby enhancing the efficiency and quality of healthcare delivery.
Learn more:
What is a PA?
Physician Assistants (PAs) are healthcare professionals who work in collaboration with physicians and other healthcare providers to deliver patient care.
Rooted in the concept of team-based care, PAs work under the supervision of licensed physicians, but they possess the autonomy to perform a wide range of clinical tasks and procedures
PA Training and Education
In Canada, the journey to becoming a Physician Assistant begins by enrolling in a PA program following undergraduate study. These programs are 2 years and students are provided a comprehensive curriculum that includes coursework, clinical rotations, and hands-on training. Throughout their training, students learn essential medical skills, such as history-taking, physical examination, diagnostics, and treatment planning.
PA Licensure and Certification
After successfully completing their education, graduates are required to pass the Physician Assistant Certification Council of Canada (PACCC) examination. This certification is essential for licensure, as PAs must be registered with the appropriate provincial or territorial regulatory body to practice.
Scope of Practice
The scope of practice for Physician Assistants in Canada varies slightly across provinces and territories. PAs conduct patient assessments, order and interpret investigations, formulate treatment plans, prescribe medications, assist in surgical procedures, and order/perform diagnostic and therapeutic procedures. See below to learn more about PA scope of practice.

PA Scope of Practice Explained
Physician Assistants' scope of practice in Canada encompasses a wide range of medical and clinical responsibilities, allowing them to provide comprehensive and patient-centred care under the supervision of licensed physicians.
The scope of practice for PAs may vary slightly across provinces and territories, but their core functions remain consistent.
Here are some key components of their scope of practice:
Patient-Focused, Culturally Competent Care: PAs are dedicated to providing patient-centred care that is respectful of each individual's cultural background, beliefs, and preferences. They establish a strong rapport with patients, ensuring open communication and active involvement in healthcare decisions. This patient-focused approach enhances patient satisfaction and overall health outcomes.
Patient Assessment: Physician Assistants are trained to conduct thorough patient assessments, which include taking detailed medical histories and performing comprehensive physical examinations. These assessments help in the accurate diagnosis and formulation of treatment plans.
Ordering and Interpreting Investigations: PAs have the authority to order and interpret various investigations, such as blood tests, imaging (x-rays, CT scan, MRI, ultrasound, etc.) and other diagnostic procedures, which aids in the timely diagnosis and treatment of patients.
Diagnosis and Treatment Planning: Physician Assistants excel in clinical reasoning and are skilled at formulating comprehensive differential diagnoses. They analyze patient data, interpret test results, and collaborate with physicians to arrive at accurate and timely diagnoses, which is crucial for initiating appropriate treatments promptly.
Prescribing Medications: Under the guidance and supervision of a licensed physician, PAs are authorized to prescribe medications to patients. This includes both ongoing prescriptions for chronic conditions and short-term medications for acute illnesses.
Procedures and Interventions: Physician Assistants are trained to perform minor medical procedures and interventions. These may include suturing wounds, administering injections, lumbar punctures, casting and reduction of fractures, joint injections, removing sutures or staples, and providing wound care.
Patient Education: PAs play a crucial role in patient education. They take the time to explain medical conditions, treatment options, and preventive measures to patients, empowering them to actively participate in their healthcare decisions.
Collaboration with Healthcare Team: Physician Assistants are adept at collaborating with various members of the healthcare team, such as nurses, pharmacists, physiotherapists, and social workers. This teamwork ensures comprehensive and coordinated care for patients.
Surgical First Assist: In some healthcare settings, PAs may assist in surgical procedures, working closely with surgeons and other surgical team members to ensure smooth and safe operations.
Medical Documentation: PAs are responsible for maintaining detailed medical documentation, including progress notes, discharge summaries, and admission orders. This ensures accurate and continuous communication between healthcare providers and supports seamless transitions of care.
On-call/Pager Responsibilities: In certain healthcare settings, PAs may have on-call or pager responsibilities, responding to urgent medical situations and providing timely medical advice and intervention.
Follow-up Care: PAs often handle follow-up care for patients after hospital discharge or medical visits. They ensure patients' progress is monitored, and any necessary adjustments to treatment plans are made.
Patient Advocacy: Physician Assistants serve as advocates for their patients, ensuring that their concerns and preferences are heard and respected. They work to address any barriers to healthcare access and promote patient well-being throughout their treatment journey.
The PA Role as explained by Practicing PAs
-

Sahand, Emergency Medicine PA
“When I actually researched the PA Profession, I saw in fact that the Physician Assistant name is almost a misnomer in that PAs are not doing clerical work or typical tasks than an “assistant” is doing, but you are a PHYSICIAN EXTENDER where you practice medicine, you see diagnose, treat illness, you prescribe medications, you assist in surgeries and perform procedures.”
-

Kimberly Scott, Orthopaedic Surgery PA
“The PA role has been extremely well received by the ER staff, nursing staff on the surgical ward, and the multiple health care providers that I provide consultations for. My supervising physicians are 100% on board with working alongside a PA.
PAs are educated in the same/similar medical model as a physician, however it is a more accelerated program. They require more precise on-the-job training.
Training a new PA grad is very similar to training an early/junior resident. If it is a PA that is new to an Orthopaedic practice or organization, the expectation is to train the PA in diagnostic imaging, Orthopaedic testing, developing a diagnosis and implementing a plan of care. Guide them to resources that they can use to learn.”
-

Harrison, Critical Care PA
“Physician Assistants are health care providers that practice medicine, first and foremost. We have different training than physicians and operate differently because of that.
PAs don’t have regulated, mandatory and formalized residencies. So even though we can work in every specialty of care, we do so in collaboration with physicians that are specialized (or not). That collaborative relationship is great because it gives us safety and flexibility, but it allows for a pretty wide range of autonomy depending on the particular PA.
It’s important for people to know that PAs are always learning and growing.
An experienced PA can do a lot, and a lot more than people expect.”
-

Dee, Acute Care Surgery PA
“There are a few differences between me (as an experienced PA) and the residents:
Junior residents rotate on the service 1-2 months at a time, as a PA I am there full time and permanent, and have built relationships with nursing staff and staff physicians of different departments. For instance, I’ll be less hesitant to get on the phone with the Interventional Radiologist when there is a specific question or a request, like inserting an urgent cholecystostomy tube for management of cholecystitis.
Residents typically prioritize time gaining surgical experience in the OR, as a PA I do occasionally assist in the OR if required, however I typically spend more time in surgical clinic, seeing consults in the emergency department and on the ward, managing patients pre- and post-op and liaising with the interprofessional team to provide quality, patient-centred care.”
-

Maitry, Radiation Oncology PA
“A PA is an extension of the physician’s role. This term has been used often, but I do find that PA’s are an extension of the entire health care team.
A physician sometimes gets bogged down with work that only they are capable of doing, whether it’s being the primary surgeon, or it’s being the radiation oncologist who has to plan their patient’s radiation treatment.
A PA can bridge the gap between the admin side of things, nursing side of things and the clinical side things.”
-

Maureen, Infectious Disease PA
“I tell people, that Physician Assistants are like the residents who never go away. So that’s really works well with physicians and nurses and other people in the healthcare profession. You have to massage that a little bit for the lay public who may not even understand what a resident is at the end of the day.
But when you think about it, and I’ve been told this by physicians that I’ve worked with in both emergency medicine as well as ID, that we reached the level of a senior resident, a very senior resident. And what’s nice about it is we provided those physicians that we work with that continuity, and they can teach us like they do residents. The main difference is that residents leave after a few weeks, while PAs stay on on the service.”
PA Education in Canada
Becoming a Physician Assistant in Canada is a rigorous and rewarding journey that prepares individuals for a critical role in the healthcare system. PA education is designed to provide aspiring healthcare professionals with the knowledge, skills, and clinical experience needed to deliver high-quality patient care under the supervision of physicians and other healthcare providers.
In Canada, the journey to becoming a Physician Assistant begins with obtaining undergraduate coursework (Bachelor’s Degree). Aspiring PAs must enroll in an accredited Physician Assistant program.
PA programs are offered programs typically last two years and combine didactic instruction with hands-on clinical training to create a well-rounded and competent healthcare professional.
PA School Year 1 (PA-S1)
1st year of PA school consists of didactic, classroom learning supplemented with hands-on clinical skills where students learn medical foundations. There is also early exposure to health care through clinical placements in the first year. This comprehensive curriculum covers essential medical sciences, clinical medicine, pharmacology, ethics, and patient communication. Students learn to perform physical examinations, interpret diagnostic tests, and develop clinical reasoning skills.
PA School Year 2 (PA-S2)
2nd year of PA school consists of clinical placements in core and elective rotations. Students gain practical experience in various medical specialties including Family Medicine, Emergency Medicine, Internal Medicine, Psychiatry, Geriatrics, Women’s Health, Paediatrics, Surgery and more. These rotations take place in hospitals, clinics, and other healthcare settings, where students work alongside healthcare professionals to apply their knowledge in real-world scenarios.
During their clinical rotations, PA students are assigned preceptors who are experienced healthcare providers. Under their guidance, students develop practical skills, enhance clinical decision-making, and gain exposure to different patient populations.
PAs practice can work in different specialties in medicinePA Lateral Mobility
One of the key strengths of Physician Assistants lies in their ability to work across a wide range of medical specialties, making them valuable assets in various healthcare settings.
Examples of PAs working in different specialties:
-
In primary care settings, PAs serve as the first point of contact for patients seeking medical attention.
They conduct patient assessments, diagnose common medical conditions, prescribe medications, and provide preventive care and health education.
PAs in primary care play a crucial role in managing chronic diseases, promoting wellness, and coordinating patient care with other healthcare providers.
-
In the Emergency Medicine department, Physician Assistants (PAs) play a critical and dynamic role in providing timely and efficient patient care. Their unique skill set and adaptability make them valuable assets in managing a wide range of medical emergencies. Here is an overview of the PA role in the Emergency Medicine department:
Patient Assessments of various undifferentiated complaints
Diagnosis and Treatment: PAs are skilled at diagnosing and managing a variety of acute medical conditions and injuries. They order and interpret diagnostic tests, such as X-rays and laboratory work, to aid in the diagnostic process. Based on their assessments, they formulate treatment plans and initiate necessary interventions.
Emergency Procedures: PAs are trained to perform a range of emergency procedures. This may include starting intravenous (IV) lines, inserting urinary catheters, suturing wounds, and stabilizing fractures or dislocations.
Medication Management: In the Emergency Medicine department, PAs can prescribe and administer medications. They are responsible for selecting appropriate medications, calculating dosages, and ensuring that patients receive the necessary pharmacological interventions promptly.
Critical Care Support: PAs play a crucial role in managing critically ill or unstable patients. They assist in the resuscitation efforts of patients experiencing life-threatening emergencies and collaborate with the medical team to stabilize and manage complex cases.
Imaging: PAs can order and interpret imaging studies, such as X-rays and CT scans, to aid in the diagnosis and decision-making process.
Patient Education and Discharge Planning: PAs take the time to educate patients and their families about their conditions, treatment options, and follow-up care. They also participate in discharge planning, ensuring that patients have appropriate instructions and resources for continued care after leaving the Emergency Medicine department.
Collaboration and Communication: PAs work closely with emergency physicians, nurses, and other healthcare professionals in a collaborative team-based approach. Effective communication is essential in rapidly assessing patients and delivering timely interventions.
Emergency Medical Protocols: PAs are well-versed in emergency medical protocols and guidelines. They adhere to evidence-based practices and follow established protocols to ensure standardized and high-quality care for all patients.
Continuous Assessment and Monitoring: Throughout a patient's stay in the Emergency Medicine department, PAs continuously assess and monitor their condition. They make informed decisions based on changes in the patient's status and adjust treatment plans accordingly.
-
In surgery and various surgical specialties, Physician Assistants (PAs) play crucial roles that contribute significantly to patient care and surgical teams' efficiency. PAs are well-trained to provide a wide range of services, working closely with surgeons and other healthcare professionals. Here's an overview of the PA role in surgery and various surgical specialties:
Outpatient Clinic: In the outpatient clinic, PAs provide specialized medical care to surgery patients during their preoperative preparation and postoperative follow-up visits. They conduct thorough preoperative assessments, review patients' medical histories, and order necessary preoperative tests to ensure patients are optimally prepared for surgery. PAs also provide postoperative care, monitoring patients' recovery progress, managing postoperative pain, and addressing any concerns or complications that may arise after surgery.
Inpatient/Ward Management: In the inpatient setting, Surgery PAs play a vital role in the management of surgery patients during their hospital stay. They conduct daily rounds, assessing surgical patients' postoperative conditions and collaborating with the surgical team to adjust treatment plans as needed. PAs work closely with the healthcare team, including surgeons, nurses, and other specialists, to coordinate comprehensive and individualized care for surgery patients.
Admitting and Discharge Planning: PAs have a role in the admission process for surgery patients, conducting thorough assessments, and collaborating with surgeons to ensure patients are medically ready for their procedures. During discharge planning, PAs work closely with the surgical team to ensure a smooth transition from the hospital to home or other care facilities for postoperative recovery. They provide detailed instructions for post-discharge care, medication management, and follow-up appointments to optimize patient recovery and outcomes.
Surgical Assist: During surgeries, PAs serve as essential members of the surgical team. They assist surgeons in various tasks, such as retracting tissues, suturing, closing incisions, and handling surgical instruments. Their support enables surgeons to focus on critical aspects of the procedure.
On-Call Responsibilities: PAs may have on-call duties, responding to urgent medical situations and providing immediate medical support to surgery patients during critical postoperative periods. During on-call hours, they are available to manage emergent postoperative needs, handle complications, and provide timely medical interventions.
Procedures: PAs with surgical expertise may assist in various surgical procedures, working closely with surgeons to support the surgical team during operations. They may perform tasks such as wound closure, tissue retraction, and suturing under the guidance and supervision of the surgical team.
-
In internal medicine, Physician Assistants (PAs) play a critical role in the diagnosis, management, and coordination of care for patients with a wide range of medical conditions. The PA role in internal medicine is diverse and multifaceted, encompassing both primary care and specialized medical care. Here are some key aspects of the PA role in internal medicine:
Patient Assessment and Diagnosis: PAs in internal medicine perform comprehensive patient assessments, including taking medical histories, conducting physical examinations, and ordering and interpreting diagnostic tests. They use their clinical expertise to diagnose medical conditions accurately and develop individualized treatment plans for patients.
Chronic Disease Management: PAs are involved in the management of chronic medical conditions such as diabetes, hypertension, asthma, and chronic obstructive pulmonary disease (COPD). They work closely with patients to develop personalized care plans, monitor disease progression, and make appropriate adjustments to treatment regimens.
Acute Illness Management: PAs provide care for patients with acute illnesses and medical conditions that require immediate attention. They manage patients with infectious diseases, respiratory infections, gastrointestinal disorders, and other acute medical issues.
Medication Management: PAs in internal medicine are authorized to prescribe medications and manage patients' medication regimens. They ensure patients receive appropriate medications, adjust dosages as needed, and monitor for potential drug interactions or side effects.
Patient Rounding: PAs participate in patient rounds, where they collaborate with the healthcare team to discuss patients' progress, treatment plans, and any changes in their medical conditions. They provide updates on their patients' status, contribute to the decision-making process, and address any concerns related to patient care.
Participating in Interprofessional Rounds: PAs actively engage in interprofessional rounds, which involve discussions with various healthcare professionals, including physicians, nurses, pharmacists, and social workers. They contribute their expertise and insights to ensure holistic and comprehensive patient care.
Family Meetings: PAs are involved in family meetings, where they communicate with patients' families about their medical conditions, treatment plans, and ongoing care. They provide a clear understanding of the patient's health status and address any questions or concerns that the family may have.
Documentation: PAs maintain accurate and detailed medical documentation of patient assessments, treatment plans, progress notes, and any changes in patient status. Clear and concise documentation is essential for effective communication within the healthcare team and for continuity of care.
Health Promotion and Preventive Care: PAs emphasize health promotion and disease prevention in internal medicine. They provide patients with education on healthy lifestyle choices, preventive screenings, and immunizations to maintain optimal health.
Coordination of Care: PAs collaborate with other healthcare providers, specialists, and allied health professionals to ensure comprehensive and coordinated care for patients. They facilitate communication among the healthcare team to optimize patient outcomes.
Admission and Discharge of Patients: PAs in internal medicine are actively involved in the admission and discharge processes of patients admitted to the hospital.
During admission, PAs conduct thorough assessments, review medical histories, and work closely with physicians to ensure patients are admitted with appropriate care plans and interventions. In the discharge planning phase, PAs collaborate with the healthcare team to ensure a smooth transition for patients from the hospital to home or other care facilities. They provide comprehensive instructions for post-discharge care, medication management, and follow-up appointments to promote optimal recovery and continuity of care.
In the discharge planning phase, PAs collaborate with the healthcare team to ensure a smooth transition for patients from the hospital to home or other care facilities. They provide comprehensive instructions for post-discharge care, medication management, and follow-up appointments to promote optimal recovery and continuity of care.
On-Call/Pager Responsibilities: PAs may have on-call or pager responsibilities, being available outside regular working hours to respond to urgent medical situations and emergencies. During on-call shifts, PAs provide immediate medical advice and intervention to address critical patient needs promptly. They collaborate with other healthcare professionals to ensure seamless patient care and support the healthcare team during urgent situations.
Complex Case Management: PAs assist in managing patients with complex medical conditions that may require multiple interventions and ongoing monitoring.
Benefits of Adding a PA
-

Improved Patient Satisfaction
PAs work in collaboration with supervising physicians, and this fosters comprehensive and personalized patient care.
Patients benefit from the expertise of both healthcare professionals, leading to enhanced patient satisfaction and better health outcomes.
-

Reduced Wait Times
With a PA on the team, the practice or department can accommodate a higher volume of patients, reducing wait times for appointments and medical services.
-

Enhanced Efficiency and Workflow
PAs are trained to perform clinical tasks, such as taking medical histories, conducting physical exams, interpreting diagnostic tests, formulating a diagnosis and differential diagnosis, formulating treatment plans, performing interventional or diagnostic procedures, prescribing medications, and engaging patient education.
This allows the healthcare team to operate more efficiently, optimizing workflow and ultimately improving overall patient management without duplicating the work.
-

Cost Savings
By delegating certain responsibilities to PAs, the practice or department can make efficient use of healthcare resources. PAs are valuable assets in managing non-complex cases, which can lead to cost savings and contribute to the overall financial sustainability of the healthcare facility.
Where PAs practice in Canada
900+ PAs are working across Canada.
At the beginning of 2023, PAs worked in 5 provinces - Alberta, Manitoba, Ontario, New Brunswick and Nova Scotia.
Towards the end of 2023, legislation and/or pilot programs were introduced in 5 more provinces including BC, Saskatchewan, Quebec, PEI and Newfoundland and Labrador.
Each province is at a different stage in integrating and regulating PAs, reflecting varied approaches to addressing healthcare system demands and workforce challenges.
The Canadian Association of Physician Assistants continues with efforts to expand the scope and recognition of PAs, with legislative changes, and the introduction of PAs in more provinces and territories.
Alberta
In 2009 the Minister of Health requested that the CPSA include PAs in the Health Professions Act as a regulated health profession and to develop a voluntary registry under the College. This was released by the college in 2010, and in 2013 the Alberta Health Services with the MOH launched a PA demonstration Project, with PAs employed in rural primary care, and urban hospital settings (e.g. surgery, internal medicine, and obstetrics).
In late 2020, Alberta passed legislation under the Health Professions Act allowing the College of Physicians and Surgeons of Alberta (CPSA) to begin regulating PAs as of April 1, 2021. This legislative change marks a critical milestone, officially recognizing PAs as regulated health professionals in Alberta. The regulation ensures that PAs follow all CPSA Standards of Practice and comply with continuing competence requirements, working under the supervision of physicians to provide a wide range of medical services.
Alberta Health Services (AHS) employs PAs in various healthcare settings, including hospitals, community clinics, emergency departments, and specialized programs like cancer care.
In April 2023, the government announced funding for the University of Calgary’s PA Program. Funding was approved in 2024, with the Calgary MPAS’ program having their inaugural class of 20 students to begin Fall 2024.
-
Government of Alberta. (2024). Health professions act. https://www.qp.alberta.ca/documents/Acts/H07.pdf
University of Calgary. (2024). UCalgary master physician assistant program funded by province. Retrieved April 25, 2024, from https://ucalgary.ca/news/ucalgary-master-physician-assistant-program-funded-province
Cumming School of Medicine. (n.d.). Physician assistant program. University of Calgary. Retrieved April 25, 2024, from https://cumming.ucalgary.ca/physician-assistant/program
College of Physicians and Surgeons of Alberta. (n.d.). Physician Assistants. Retrieved June 11, 2024, from https://cpsa.ca/physician-assistants/
Government of Alberta. (2023, March 31). Physicians, Surgeons, Osteopaths and Physician Assistants Profession Regulation. Retrieved June 11, 2024, from https://open.alberta.ca/publications/2020_200
Alberta Health Services. (n.d.). Physician Assistant (PA). Retrieved June 11, 2024, from https://www.albertahealthservices.ca/
Canadian Association of Physician Assistants. (n.d.). Legislation. Retrieved June 11, 2024, from https://capa-acam.ca/pa-facts/
British Columbia
In 2023, BC took substantial steps toward licensing and regulating PAs. The Health Professions and Occupations Act (HPOA), passed in 2022, set the groundwork for this integration. This act aims to modernize the framework within which health profession regulatory colleges operate, ensuring better governance and improved efficiency across the health professions in BC.
In April 2023, during the budget estimates process, BC’s Health Minister Adrian Dix confirmed that the College of Physicians and Surgeons of BC (CPSBC) was actively working on the policy framework for licensing and regulating PAs. This move is expected to address the province's healthcare workforce challenges, particularly in rural and underserved areas.
British Columbia's Ministry of Health has enacted a bylaw permitting Physician Assistants (PAs) to work in emergency departments as of October 25, 2023. This decision was prompted by the need to address staffing difficulties and the closure of emergency rooms.
In February 2024, Island Health announced the hiring of the first PA at Saanich Peninsula Hospital as part of a pilot project to boost ER services in collaboration with 24/7 OEMS. Saanich Peninsula Hospital Emergency Department is recruiting up to five Physician Assistants (PAs). Each health authority in British Columbia is assessing healthcare sites to determine priority areas for PA deployment.
While BC does not currently have a PA training program, there are ongoing discussions and efforts to develop educational pathways for PAs within the province. The Canadian Association of Physician Assistants (CAPA) and other stakeholders are advocating for the establishment of PA education programs to ensure a steady supply of qualified PAs to meet the growing demand.
-
Tunney, C. (2024). Bylaw change could see more physician assistants in B.C. CBC News. Retrieved April 25, 2024, from https://www.cbc.ca/news/canada/british-columbia/bylaw-change-physician-assistants-1.6981706
Doctors of BC. (2024). Including physician assistants in BC health care system. Retrieved April 25, 2024, from https://www.doctorsofbc.ca/news/including-physician-assistants-bc-health-care-system
Island Health. (n.d.). Island Health hiring physician assistant at Saanich Peninsula Hospital under new provincial pilot project. CHEK News. Retrieved April 25, 2024, from https://www.cheknews.ca/island-health-hiring-physician-assistant-at-saanich-peninsula-hospital-under-new-provincial-pilot-project-1192845/
Government of British Columbia. (2023, September 27). Physician assistants are one step closer to joining B.C.’s health-care workforce. Retrieved June 11, 2024, from https://news.gov.bc.ca/
College of Physicians and Surgeons of BC. (n.d.). Physician Assistants. Retrieved June 11, 2024, from https://www.cpsbc.ca/
BC Rural Health Network. (2023, April 30). Physician Assistants Take First Steps Toward Licensing and Regulation in British Columbia. Retrieved June 11, 2024, from https://bcruralhealth.org/
Manitoba
The journey of PAs in Manitoba began with the enactment of legislation in 1999, which regulated PAs under the title of Clinical Assistants - Certified. This initial step allowed for the licensing and practice of PAs within the province. In 2009, a significant amendment to the Manitoba Medical Act established a separate PA registry and formally recognized the title and practice of Physician Assistants. This amendment provided PAs with a distinct professional identity and a defined scope of practice under the College of Physicians and Surgeons of Manitoba (CPSM).
Manitoba is home to one of Canada's pioneering PA education programs. In 2008, the University of Manitoba welcomed its first class of PA students into the Manitoba Master of PA Studies. This program, which offers a Master’s level degree, was developed in partnership with the faculties of Graduate Studies and Medicine. It stands as the first Master’s level PA program in Canada, designed to meet high academic and clinical standards.
Today, nearly 150 PAs practice in Manitoba across various medical and surgical specialties, contributing significantly to the healthcare system. PAs in Manitoba work closely with supervising physicians and multidisciplinary teams to provide efficient, high-quality care, especially in primary care, emergency medicine, long-term care, and specialized medical fields.
The establishment of the Physician and Clinical Assistants of Manitoba (PCAM) further strengthens the profession by representing PAs and Clinical Assistants across the province. PCAM advocates for the profession, supports ongoing education, and ensures the maintenance of high ethical standards in practice.
-
Health Careers Manitoba. (n.d.). Physician assistants. Retrieved April 25, 2024, from https://healthcareersmanitoba.ca/professions/physician-and-clinical-assistants/physician-assistants/
Canadian Association of Physician Assistants. (n.d.). History. Retrieved June 11, 2024, from https://capa-acam.ca/about/history
Canadian Association of Physician Assistants. (n.d.). Legislation. Retrieved June 11, 2024, from https://capa-acam.ca/about/legislation
Canadian Association of Physician Assistants. (2023, November 24). Unveiling the Impact of Physician Assistants in Manitoba's Healthcare System. Retrieved June 11, 2024, from https://capa-acam.ca/news/unveiling-the-impact-of-physician-assistants-in-manitobas-healthcare-system
Physician and Clinical Assistants of Manitoba. (n.d.). About PCAM. Retrieved June 11, 2024, from https://pcam.ca
Nova Scotia
In 2019, Nova Scotia announced a pilot project to introduce PAs into the province. In January 2020, three Physician Assistants joined Orthopaedic Surgery as part of a pilot project in Nova Scotia.
In October 2021, he first reading of the Physician Assistant Act was passed in Halifax, giving the Minister of Health authority to make regulations around PAs.
This marked a crucial step in formally recognizing and regulating the PA profession in the province. This legislation is part of broader efforts to modernize the healthcare system and better integrate PAs.
A significant milestone in PA education in Nova Scotia is the establishment of the Master of Physician Assistant Studies (MPAS) program at Dalhousie University. Announced in 2023, this two-year program began January 2024 and is the first PA program in Atlantic Canada. The program aims to address the critical need for healthcare providers in the province, particularly in rural and underserved areas. The inaugural class consists of 24 students, with priority given to Nova Scotian applicants.
-
Nova Scotia Health. (2024a). Physician assistant role in pilot program aims to help improve access to hip and knee replacement. Retrieved April 25, 2024, from https://www.nshealth.ca/news/physician-assistant-role-pilot-program-aims-help-improve-access-hip-and-knee-replacement
Nova Scotia Health. (2024b). A day in the life of one of Nova Scotia Health's first physician assistants. Retrieved April 25, 2024, from http://www.nshealth.ca/news/day-life-one-nova-scotia-healths-first-physician-assistants
Nova Scotia Legislature. (2024). Bill No. 188. Retrieved April 25, 2024, from https://nslegislature.ca/legc/bills/63rd_2nd/1st_read/b188.htm
Government of Nova Scotia. (2023, August 3). New Master’s Program to Train Physician Assistants. Retrieved June 11, 2024, from https://novascotia.ca/news/release/?id=20230803004
Canadian Association of Physician Assistants. (2024, January 2). New Physician Assistant Training Program at Dalhousie will help address Health Workforce Challenges. Retrieved June 11, 2024, from https://capa-acam.ca/news/new-training-program-at-dalhousie-will-help-address-health-workforce-challenges
Cision PR Newswire. (2021, October 15). Physician Assistants Act in Nova Scotia Important Step in Health Modernization. Retrieved June 11, 2024, from https://www.newswire.ca/news-releases/physician-assistants-act-in-nova-scotia-important-step-in-health-modernization-847551751.html
Nova Scotia Health Authority. (2023, August 3). New Master’s Program to Train Physician Assistants. Retrieved June 11, 2024, from https://physicians.nshealth.ca/news/new-masters-program-train-physician-assistants
Newfoundland and Labrador
In October 2022, a plan for the introduction of PAs was announced by the Newfoundland Minister of Health. n November 2023, Newfoundland and Labrador launched a 3 year PA pilot program to introduce PAs into the province’s healthcare system. This had PAs work in each of the 5 health zones, in different healthcare settings including inpatient care, surgery, hospitalist coverage, orphaned patient follow-up reports, ED and primary care.
This development is part of broader efforts by the Atlantic provinces to address healthcare workforce challenges. The Canadian Association of Physician Assistants (CAPA) has been actively advocating for the integration of PAs across the region to enhance healthcare delivery and ensure better patient outcomes.
The introduction of PAs is expected to have a positive impact on the healthcare system in Newfoundland and Labrador, especially in underserved rural communities. By increasing the number of healthcare providers, the province aims to improve in-person care, reduce reliance on virtual care, and increase preventive health measures such as cancer screening
-
Government of Newfoundland and Labrador. (2019, July 29). New Public Health Legislation Now Law in Newfoundland and Labrador. Retrieved June 11, 2024, from https://www.gov.nl.ca/releases/2019/health/0729n02/
Canadian Association of Physician Assistants. (2023, November 6). 10 PAs coming to Newfoundland and Labrador to aid overworked doctors. Retrieved June 11, 2024, from https://capa-acam.ca/advocacy/press-releases/atlantic-provinces-call-on-physician-assistants-to-help-with-health-workforce-challenges-2023-04-05
Canadian Association of Physician Assistants. (2023, April 5). Atlantic Provinces Call on Physician Assistants to Help with Health Workforce Challenges. Retrieved June 11, 2024, from https://capa-acam.ca/advocacy/press-releases/atlantic-provinces-call-on-physician-assistants-to-help-with-health-workforce-challenges-2023-04-05
New Brunswick
The inclusion of PAs in New Brunswick's healthcare system began in 2009 when the College of Physicians and Surgeons of New Brunswick (CPSNB) amended the New Brunswick Medical Act to include PAs. This legislation allowed for the licensing of PAs, enabling them to practice under the supervision of physicians and contribute significantly to the province's healthcare services.
New Brunswick has been proactive in integrating PAs into its healthcare teams, particularly through pilot programs aimed at demonstrating their value. One of the most notable pilot projects took place at Dr. Everett Chalmers Regional Hospital in Fredericton, where PAs were introduced to assist with surgical services. The success of this program led to its permanent establishment, showcasing the crucial role PAs play in improving patient care and reducing wait times.
New Brunswick's commitment to expanding the PA profession is part of a broader strategy to address healthcare workforce challenges. The province continues to advocate for the increased utilization of PAs to enhance access to care, particularly in underserved areas
-
MacKay, F & Dickson, K. (2024, April 25). CAPA Webinar: Emergency Medicine Dr. Everett Chalmers Regional Hospital, Fredericton, NB [Webinar] https://capa-acam.ca/events/enhancing-healthcare-exploring-the-role-of-physician-assistants-april-25th-2024-04-25
Canadian Association of Physician Assistants. (2023, April 5). Atlantic Provinces Call on Physician Assistants to Help with Health Workforce Challenges. Retrieved June 11, 2024, from https://capa-acam.ca/advocacy/press-releases/atlantic-provinces-call-on-physician-assistants-to-help-with-health-workforce-challenges-2023-04-05
Canadian Association of Physician Assistants. (n.d.). PA Facts. Retrieved June 11, 2024, from https://capa-acam.ca/pa-facts
Canadian Association of Physician Assistants. (2023, November 6). 10 PAs coming to Newfoundland and Labrador to aid overworked doctors. Retrieved June 11, 2024, from https://capa-acam.ca/advocacy/press-releases/atlantic-provinces-call-on-physician-assistants-to-help-with-health-workforce-challenges-2023-04-05
Ontario
In 2006 the Ontario Ministry of Health and Long-Term care announced the introduction of PAs into its province, with the start of the Ontario PA Demonstration Project in 2007. This project aimed to integrate PAs into various clinical settings to evaluate their impact on the healthcare system. The success of this initiative paved the way for further legislative developments.
On April 27, 2021, Ontario’s Minister of Health introduced legislation, once passed, to regulate PAs in Ontario. On June 3, 2021 Bill 283 Advanced Oversight and Planning in Ontario’s Health System Act received Royal Assent.
Regulation of PAs in Ontario will be through the College of Physicians and Surgeons of Ontario (CPSO). In 2021, Ontario introduced legislation to bring PAs under the regulatory authority of the College of Physicians and Surgeons of Ontario (CPSO). CPSO will begin regulating PAs starting April 1, 2025. The regulation ensures title protection, and that PAs can only perform controlled acts through delegation by a supervising physician, maintaining a high standard of care and accountability.
This move aligns Ontario with other provinces like Manitoba, New Brunswick, and Alberta, which also regulate PAs under their respective medical regulators.
Ontario is home to two PA education programs. McMaster University offers the Physician Assistant Education Program, which was established in 2008, and the University of Toronto launched its Physician Assistant Professional Degree Program in 2010. These programs are designed to equip students with the necessary skills and knowledge to perform effectively as PAs within the healthcare system. Both programs are highly regarded and contribute to the growing number of certified PAs in the province
-
Canadian Association of Physician Assistants. (2021). Regulation of PAs in Ontario: Important step in health modernization. Retrieved April 25, 2024, from https://capa-acam.ca/2021/04/regulation-of-pas-in-ontario-important-step-in-health-modernization/
College of Physicians and Surgeons of Ontario. (2024). Physician assistants. Retrieved from https://www.cpso.on.ca/en/Physician-Assistants
Elliott, C. [@celliottability]. (2021, June 3). Excited to announce that Ontario is moving forward with regulating physician assistants [Tweet]. Twitter. https://twitter.com/celliottability/status/1400571891820253184
College of Physicians and Surgeons of Ontario. (2021, June 28). CPSO to regulate physician assistants. Retrieved April 25, 2024, from https://dialogue.cpso.on.ca/2021/06/cpso-to-regulate-physician-assistants/
HealthForceOntario. (n.d.). Physician Assistants. Retrieved June 11, 2024, from https://www.healthforceontario.ca/en/Home/Health_Providers/Physician_Assistants
Prince Edward Island (PEI)
The PEI Government and College of Physicians and Surgeons of PEI, and Health PEI In June 2023, new regulations under the Regulated Health Professions Act were enacted, allowing Physician Assistants to practice in PEI. This legislative move is part of broader efforts to address healthcare workforce challenges and improve patient access to care. The regulations establish a new class of registration for PAs under the College of Physicians and Surgeons of PEI, enabling them to perform a variety of medical tasks under the direct supervision of licensed physicians
PEI has been actively recruiting PAs to join Health PEI, the provincial health authority. This initiative includes hiring five PAs to work across various medical settings, such as primary care, emergency medicine, and surgery.
-
Government of Prince Edward Island. (n.d.). Associate physicians and physician assistants added to health care system. Retrieved April 25, 2024, from https://www.princeedwardisland.ca/en/news/associate-physicians-and-physician-assistants-added-to-health-care-system
Health PEI. (2023, November 3). Moving forward toward welcoming physician assistants. Retrieved April 25, 2024, from https://src.healthpei.ca/note-michael-nov-3-2023-moving-forward-toward-welcoming-physician-assistants
Government of Prince Edward Island. (n.d.). Hiring information for physician assistants. Retrieved April 25, 2024, from https://www.princeedwardisland.ca/en/information/health-and-wellness/hiring-information-for-physician-assistants
Government of Prince Edward Island. (2023, June 16). Physician Assistants Regulations. Retrieved June 11, 2024, from https://www.princeedwardisland.ca/en/information/health-and-wellness/physician-assistants-regulations
Government of Prince Edward Island. (2023, November 3). Province recruiting physician assistants to join health care system. Retrieved June 11, 2024, from https://www.princeedwardisland.ca/en/news/province-recruiting-physician-assistants-to-join-health-care-system
Government of Prince Edward Island. (2023, June 15). Associate Physicians and Physician Assistants added to health care system. Retrieved June 11, 2024, from https://www.princeedwardisland.ca/en/news/associate-physicians-and-physician-assistants-added-to-health-care-system
Canadian Association of Physician Assistants. (n.d.). PA Facts. Retrieved June 11, 2024, from https://capa-acam.ca/pa-facts
Saskatchewan
The Medical Professional Amendment Act, 2023 includes legislative changes to allow PAs to practice in the province, and be regulated under the College of Physicians and Surgeons of Saskatchewan. Physician Assistants were introduced to Saskatchewan in early 2023 with plans for integration in different healthcare settings including primary care, long-term care, ER, oncology, GIM and surgery.
The government of Saskatchewan recently announced that the University of Saskatchewan’s College of Medicine will be establishing a 2 year Masters PA program with 20 seats, to start Fall 2025. This program will initially accommodate 20 students and is designed to meet the specific healthcare needs of the province, particularly in rural and remote areas.
These initiatives are part of a broader strategy to bolster the healthcare workforce in Saskatchewan, with significant investments in recruitment, training, and retention of healthcare professionals.
-
Legislative Assembly of Saskatchewan. (2023). Bill 129: An Act to License Physician Assistants. Retrieved April 25, 2024, from https://docs.legassembly.sk.ca/legdocs/Bills/29L3S/Bill29-129.pdf
Government of Saskatchewan. (2023, March 30). Saskatchewan introduces legislation to license physician assistants. Retrieved April 25, 2024, from https://www.saskatchewan.ca/government/news-and-media/2023/march/30/saskatchewan-introduces-legislation-to-license-physician-assistants
Government of Saskatchewan. (2023, October 31). Physician assistant training program to proceed. Retrieved April 25, 2024, from https://www.saskatchewan.ca/government/news-and-media/2023/october/31/physician-assistant-training-program-to-proceed
Government of Saskatchewan. (n.d.). Physician Assistants. Retrieved June 11, 2024, from https://www.saskatchewan.ca/residents/health/health-human-resources/physician-assistants
Saskatchewan Health Authority. (n.d.). Physician Assistant. Retrieved June 11, 2024, from https://www.healthcareersinsask.ca/pa/
Canadian Armed Forces
Military PAs can be stationed across Canada (including remote places such as the North Pole), as well as overseas and in the navy. Canada PAs have a long history in the Canadian armed forces (CAF), and the term ‘Physician Assistant’ was first used in 1984 to describe senior medics. In 2002, a 2 year PA Education program is re-designed and launched by the CAF. This was accredited in 2004. In 2016 PAs were commissioned to officer status.
Learn more about PAs in Canada from the Canadian Association of Physician Assistants (CAPA)
The Canadian Association of Physician Assistants (CAPA) is a national professional association that advocates for PAs and PA students.
References and Resources
PA Programs:
Canadian Association of Physician Assistants (CAPA)
From Health Organizations
College of Physicians and Surgeons of Ontario (CPSO): Delegation of Controlled Acts
College of Physicians and Surgeons of Manitoba: Physician Assistant (Regular Associate Member)
College of Pharmacists of Manitoba: Clinical and Physician Assistant: Prescribing Authority
Ontario College of Pharmacists: Ontario’s Physician Assistants: An Update
From Canadian PA/PA-Student Organizations
Journal of Canada’s Physician Assistants (JCanPA)
Conference Board of Canada Studies
PDFs free to download with free registration
Value of Physician Assistants: Understanding the Role of Physician Assistants Within Health Systems
Gaining Efficiency: Increasing the Use of Physician Assistants in Canada
Other Studies and Papers about PAs in Canada:
Bohm, E. R., Dunbar, M., Pitman, D., Rhule, C., & Araneta, J. (2010). Experience with physician assistants in a Canadian arthroplasty program. Canadian journal of surgery. Journal canadien de chirurgie, 53(2), 103–108.
Bowen, S., et al. (2016). Potential of physician assistants to support primary care: Evaluating their introduction at 6 primary care and family medicine sites. Canadian Family Physician, 62(5), e268–e277.
Burrows, K. Vanstone, M. & Jones I. Physician Assistants, Introduction to the Health Workforce in Canada.
Decloe, M., McCready, J., Downey, J., & Powis, J. (2015). Improving health care efficiency through the integration of a physician assistant into an infectious diseases consult service at a large urban community hospital. The Canadian journal of infectious diseases & medical microbiology, 26(3), 130–132.
Fréchette, D; Shrichand, A. Insights into the physician assistant profession in Canada, JAAPA: July 2016 – Volume 29 – Issue 7 – p 35-39
Johal, J., & Dodd, A. (2017). Physician extenders on surgical services: a systematic review. Canadian journal of surgery. 60(3), 172–178.
Jones, I; St-Pierre, N. Physician assistants in Canada, JAAPA: March 2014 – Volume 27 – Issue 3 – p 11-13
Jones, I. W., & Hooker, R. S. (2011). Physician assistants in Canada: update on health policy initiatives. Canadian family physician 57(3), e83–e88.
Mertens, J; Descoteaux, M. The evolution of PAs in the Canadian Armed Forces, JAAPA: January 2017 – Volume 30 – Issue 1 – p 1-6
Taylor MT et al. Qualitative study of employment of physician assistants by physicians: benefits and barriers in the Ontario health care system. Can Fam Physician. 2013;59(11):e507-13.