What is a PA?
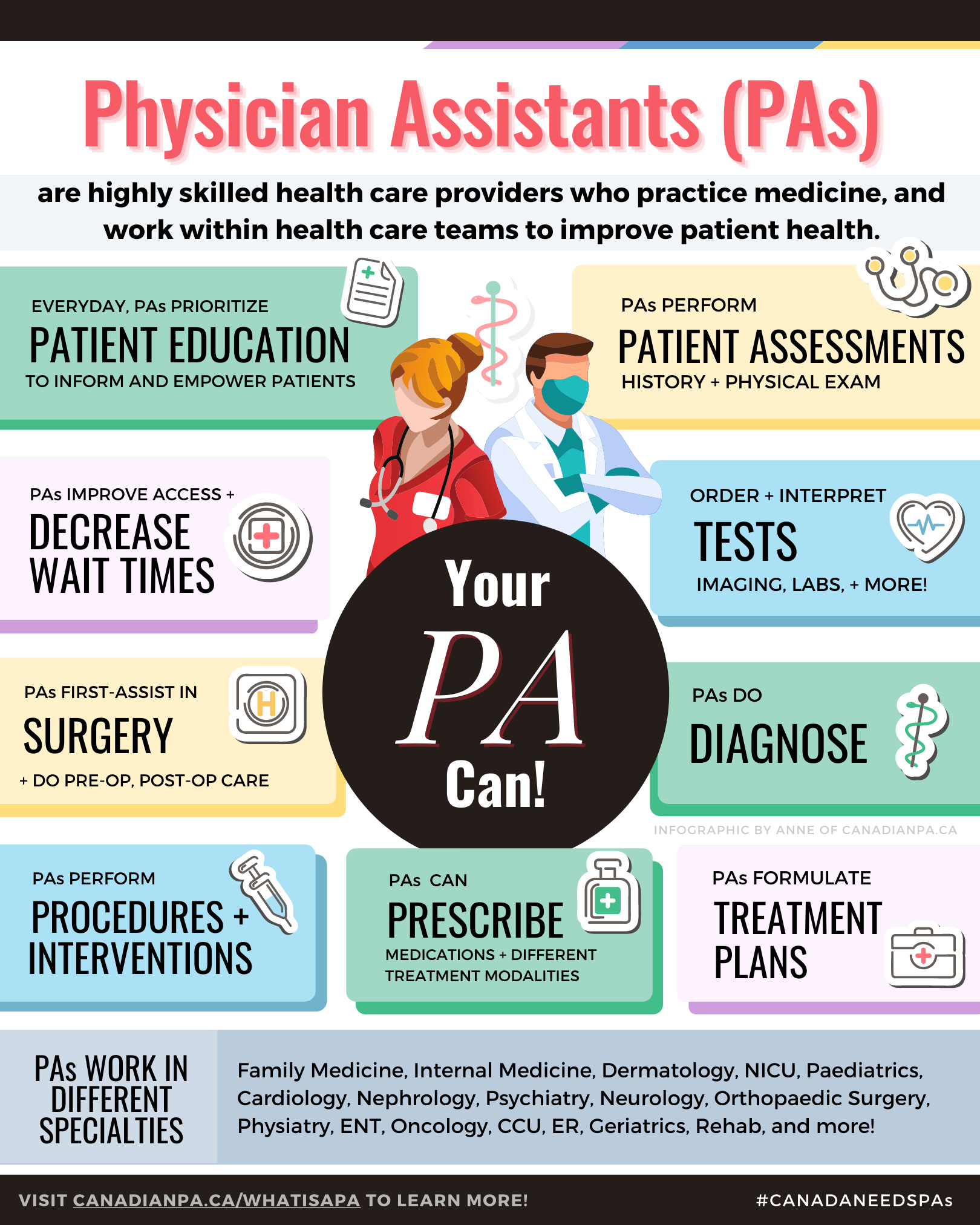
Physician Assistants (PAs) are healthcare professionals who work in collaboration with physicians and other healthcare providers to deliver patient care.
Rooted in the concept of team-based care, PAs work under the supervision of licensed physicians, but they possess the autonomy to perform a wide range of clinical tasks and procedures.
PA Education
PA programs are offered programs typically last two years and combine didactic instruction with hands-on clinical training to create a well-rounded and competent healthcare professional.
PA School Year 1 (PA-S1)
1st year of PA school consists of didactic, classroom learning supplemented with hands-on clinical skills where students learn medical foundations. There is also early exposure to health care through clinical placements in the first year. This comprehensive curriculum covers essential medical sciences, clinical medicine, pharmacology, ethics, and patient communication. Students learn to perform physical examinations, interpret diagnostic tests, and develop clinical reasoning skills.
PA School Year 2 (PA-S2)
2nd year of PA school consists of clinical placements in core and elective rotations. Students gain practical experience in various medical specialties including Family Medicine, Emergency Medicine, Internal Medicine, Psychiatry, Geriatrics, Women’s Health, Paediatrics, Surgery and more. These rotations take place in hospitals, clinics, and other healthcare settings, where students work alongside healthcare professionals to apply their knowledge in real-world scenarios.
During their clinical rotations, PA students are assigned preceptors who are experienced healthcare providers. Under their guidance, students develop practical skills, enhance clinical decision-making, and gain exposure to different patient populations.
Becoming PA Certified
In Canada, Physician Assistants (PAs) are certified through the Physician Assistant Certification Council of Canada (PACCC). This certification is essential for PAs to practice in Canada and demonstrates that they meet the national standards for competency and practice in the profession
-
Candidates must graduate from a Physician Assistant program that is accredited by the Canadian Medical Association’s Conjoint Accreditation Services (or an equivalent recognized by PACCC). In Canada, there are a few key programs, such as those offered by:
View Overview of PA Programs where we cover stats, class sizes, curriculum overview and admission requirements.
-
After completing the PA program, graduates must pass the PA Certification Examination (PACE) administered by PACCC. This exam is typically offered once a year and tests the candidate's knowledge and skills across various areas of medical practice.
The exam is comprehensive, covering topics like clinical medicine, diagnostics, therapeutics, and professional practice.
-
Upon passing the certification exam, candidates are awarded the Canadian Certified Physician Assistant (CCPA) designation. This credential signifies that the individual has met the national standards for entry-level PA practice in Canada.
-
Continuing Professional Development (CPD): CCPAs must participate in ongoing professional development to maintain their certification. This includes completing a minimum of 40 CPD credits every two years.
Certification Renewal: The CCPA designation must be renewed every five years, which includes demonstrating ongoing professional development and maintaining a current practice.
PA Scope of Practice
PA scope of practice in Canada encompasses a wide range of medical and clinical responsibilities, allowing provision of comprehensive and patient-centred care in collaboration with a supervising physician.
-
PAs are trained to approach patient assessments with strong clinical reasoning and attention to detail.
They gather key information through focused history-taking and physical exams, interpret test results, and use that data to understand what might be causing a patient’s symptoms.
This process allows them to form a clear, accurate picture of the issue and contribute meaningfully to timely diagnosis and care planning
-
PAs are qualified to order and interpret a wide range of diagnostic tests, including blood work, imaging studies (such as X-rays, CT scans, MRIs, and ultrasounds), and other investigative procedures.
This capability supports timely clinical decision-making and helps ensure patients receive accurate diagnoses and appropriate treatment without unnecessary delays.
-
PAs are trained in the medical model, using clinical reasoning (the ability to assess symptoms, interpret test results, and apply medical knowledge to make informed decisions).
They use this skill to form accurate diagnoses and treatment plans, working closely with physicians to ensure patients receive timely and appropriate care.
-
PAs are authorized to prescribe medications to patients in collaboration with a supervising physician.
This includes both ongoing prescriptions for chronic conditions and short-term medications for acute illnesses.
-
Physician Assistants are trained to perform medical procedures and interventions.
These may include suturing wounds, administering injections, lumbar punctures, casting and reduction of fractures, joint injections, removing sutures or staples, and providing wound care.
-
PAs often serve as surgical assistants, working directly with surgeons during procedures to help ensure safe, efficient operations.
This includes tasks like handling instruments, maintaining a clear surgical field, closing incisions, and supporting the team throughout the surgery.
-
PAs may take on-call or pager duties, where they respond to requests from other health care teams in hospital, addressing urgent medical issues as they arise.
When paged, the PA assesses the patient, addresses the concern, and provides recommendations to the referring team.
Specialties That Employ PAs
One of the key strengths of Physician Assistants lies in their flexibility to work across a wide range of medical specialties and clinical settings.
-
Physician Assistants are known for their flexibility and versatility in clinical practice. Trained as generalists, PAs can work across a wide range of specialties—from emergency medicine and orthopaedics to dermatology and psychiatry. With the ability to transition between disciplines without retraining, PAs bring adaptable, team-based care to wherever patients need them most
-
Family Medicine
Emergency Medicine
Surgery
Pediatrics
Internal Medicine
Orthopaedic Surgery
Dermatology
Psychiatry
Cardiology
Oncology
Geriatrics
Obstetrics and Gynecology (OB/GYN)
Nephrology
Neurology
Endocrinology
Urology
Pulmonology
Gastroenterology
Infectious Disease
Rheumatology
Hematology
Pain Management
Occupational Medicine
Physical Medicine and Rehabilitation (PM&R)
Radiology
Plastic Surgery
ENT (Ear, Nose, and Throat)
Allergy and Immunology
Sports Medicine
Palliative Care/Hospice
-
Lateral Mobility
Lateral mobility refers to the ability of Physician Assistants (PAs) to move between different medical specialties during their careers. Unlike some healthcare professionals who are often trained and restricted to a single specialty, PAs have the flexibility to switch fields without needing to undergo entirely new formal education.
This is because PAs are trained in a broad, general medical model that equips them with the foundational knowledge and skills to work in various areas of medicine. For example, a PA who starts their career in emergency medicine could later transition to dermatology or orthopaedics with additional on-the-job training and experience.
This flexibility is a significant advantage of the PA profession, allowing PAs to pursue different interests and respond to changing healthcare needs throughout their careers.
PA Practice in Canada
Each province is at a different stage in integrating and regulating PAs, reflecting varied approaches to addressing healthcare system demands and workforce challenges.
The Canadian Association of Physician Assistants continues with efforts to expand the scope and recognition of PAs, with legislative changes, and the introduction of PAs in more provinces and territories.
-
In 2009, Alberta’s Minister of Health asked the College of Physicians and Surgeons of Alberta (CPSA) to recognize Physician Assistants (PAs) as a regulated health profession under the Health Professions Act. A voluntary registry was introduced in 2010, and by 2013, Alberta Health Services and the Ministry of Health launched a PA Demonstration Project, placing PAs in both rural primary care and urban hospital settings such as surgery, internal medicine, and obstetrics.
A major shift came in late 2020, when new legislation officially gave CPSA the authority to regulate PAs. This took effect on April 1, 2021, making Alberta the first province to formally regulate the profession. Under this model, PAs must meet CPSA’s Standards of Practice and continuing competency requirements, while working under physician supervision to deliver a broad range of medical services.
Today, Alberta Health Services employs PAs in hospitals, clinics, emergency departments, and specialized areas like oncology. In 2023, the provincial government committed funding for the University of Calgary’s PA program. The program was approved in 2024, with its first cohort of 20 students starting that fall.
References
Government of Alberta. (2024). Health professions act. https://www.qp.alberta.ca/documents/Acts/H07.pdf
University of Calgary. (2024). UCalgary master physician assistant program funded by province. Retrieved April 25, 2024, from https://ucalgary.ca/news/ucalgary-master-physician-assistant-program-funded-province
Cumming School of Medicine. (n.d.). Physician assistant program. University of Calgary. Retrieved April 25, 2024, from https://cumming.ucalgary.ca/physician-assistant/program
College of Physicians and Surgeons of Alberta. (n.d.). Physician Assistants. Retrieved June 11, 2024, from https://cpsa.ca/physician-assistants/
Government of Alberta. (2023, March 31). Physicians, Surgeons, Osteopaths and Physician Assistants Profession Regulation. Retrieved June 11, 2024, from https://open.alberta.ca/publications/2020_200
Alberta Health Services. (n.d.). Physician Assistant (PA). Retrieved June 11, 2024, from https://www.albertahealthservices.ca/
Canadian Association of Physician Assistants. (n.d.). Legislation. Retrieved June 11, 2024, from https://capa-acam.ca/pa-facts/
-
In 2023, British Columbia made meaningful progress toward licensing and regulating Physician Assistants (PAs). Building on the 2022 Health Professions and Occupations Act (HPOA), which modernizes how health professions are governed, the province began developing a policy framework through the College of Physicians and Surgeons of BC (CPSBC). This initiative aims to strengthen the healthcare system, particularly in rural and underserved areas.
In October 2023, the Ministry of Health enacted a bylaw allowing PAs to work in emergency departments. The decision responded to ongoing ER staffing challenges and temporary closures. Soon after, Island Health hired its first PA at Saanich Peninsula Hospital as part of a pilot project with 24/7 OEMS. Up to five PAs are being recruited for that site, and other health authorities across BC are now identifying priority locations for PA integration.
While BC doesn’t yet offer a PA training program, discussions are underway to build local education pathways. Organizations like the Canadian Association of Physician Assistants (CAPA) continue to advocate for expanding training opportunities to meet growing demand across the province.
References:
Tunney, C. (2024). Bylaw change could see more physician assistants in B.C. CBC News. Retrieved April 25, 2024, from https://www.cbc.ca/news/canada/british-columbia/bylaw-change-physician-assistants-1.6981706
Doctors of BC. (2024). Including physician assistants in BC health care system. Retrieved April 25, 2024, from https://www.doctorsofbc.ca/news/including-physician-assistants-bc-health-care-system
Island Health. (n.d.). Island Health hiring physician assistant at Saanich Peninsula Hospital under new provincial pilot project. CHEK News. Retrieved April 25, 2024, from https://www.cheknews.ca/island-health-hiring-physician-assistant-at-saanich-peninsula-hospital-under-new-provincial-pilot-project-1192845/
Government of British Columbia. (2023, September 27). Physician assistants are one step closer to joining B.C.’s health-care workforce. Retrieved June 11, 2024, from https://news.gov.bc.ca/
College of Physicians and Surgeons of BC. (n.d.). Physician Assistants. Retrieved June 11, 2024, from https://www.cpsbc.ca/
BC Rural Health Network. (2023, April 30). Physician Assistants Take First Steps Toward Licensing and Regulation in British Columbia. Retrieved June 11, 2024, from https://bcruralhealth.org/
-
Manitoba was one of the first provinces in Canada to formally recognize and regulate Physician Assistants (PAs), initially under the title “Clinical Assistant – Certified” in 1999. In 2009, key amendments to the Manitoba Medical Act established a dedicated PA registry and formally recognized the PA role and scope of practice under the College of Physicians and Surgeons of Manitoba (CPSM).
The University of Manitoba launched Canada’s first Master’s-level PA program in 2008, admitting 15 students. Developed with the Faculties of Graduate Studies and Medicine, the program doubled its intake in 2024 and remains a national leader in PA education.
Today, nearly 150 PAs work across Manitoba in specialties such as emergency medicine, primary care, long-term care, and surgery. They contribute to timely, collaborative care throughout the province.
The Physician and Clinical Assistants of Manitoba (PCAM) serves as the professional body for PAs and Clinical Assistants. PCAM supports advocacy, continuing education, and the advancement of ethical, high-quality practice.
References:
Canadian Association of Physician Assistants. (2024, October 18). Update from 2024 CAPA Annual Members Meeting. Ottawa, ON.
Health Careers Manitoba. (n.d.). Physician assistants. Retrieved April 25, 2024, from https://healthcareersmanitoba.ca/professions/physician-and-clinical-assistants/physician-assistants/
Canadian Association of Physician Assistants. (n.d.). History. Retrieved June 11, 2024, from https://capa-acam.ca/about/history
Canadian Association of Physician Assistants. (n.d.). Legislation. Retrieved June 11, 2024, from https://capa-acam.ca/about/legislation
Canadian Association of Physician Assistants. (2023, November 24). Unveiling the Impact of Physician Assistants in Manitoba's Healthcare System. Retrieved June 11, 2024, from https://capa-acam.ca/news/unveiling-the-impact-of-physician-assistants-in-manitobas-healthcare-system
Physician and Clinical Assistants of Manitoba. (n.d.). About PCAM. Retrieved June 11, 2024, from https://pcam.ca
-
In 2019, Nova Scotia launched a pilot project to introduce PAs into the province’s healthcare system. By January 2020, three PAs began working in Orthopaedic Surgery as part of this initiative. Progress continued with the first reading of the Physician Assistant Act in October 2021, granting the Minister of Health the authority to create regulations for the profession—a key step toward formal recognition and regulation of PAs in the province.
A major advancement in PA education followed with the announcement of the Master of Physician Assistant Studies (MPAS) program at Dalhousie University in 2023. The two-year program officially began in January 2024, marking the first PA program in Atlantic Canada. With an inaugural class of 24 students and priority admission for Nova Scotians, the program is designed to help meet healthcare needs, especially in rural and underserved communities.
References:
Canadian Association of Physician Assistants. (2024, October 18). Update from 2024 CAPA Annual Members Meeting. Ottawa, ON.
Nova Scotia Health. (2024a). Physician assistant role in pilot program aims to help improve access to hip and knee replacement. Retrieved April 25, 2024, from https://www.nshealth.ca/news/physician-assistant-role-pilot-program-aims-help-improve-access-hip-and-knee-replacement
Nova Scotia Health. (2024b). A day in the life of one of Nova Scotia Health's first physician assistants. Retrieved April 25, 2024, from http://www.nshealth.ca/news/day-life-one-nova-scotia-healths-first-physician-assistants
Nova Scotia Legislature. (2024). Bill No. 188. Retrieved April 25, 2024, from https://nslegislature.ca/legc/bills/63rd_2nd/1st_read/b188.htm
Government of Nova Scotia. (2023, August 3). New Master’s Program to Train Physician Assistants. Retrieved June 11, 2024, from https://novascotia.ca/news/release/?id=20230803004
Canadian Association of Physician Assistants. (2024, January 2). New Physician Assistant Training Program at Dalhousie will help address Health Workforce Challenges. Retrieved June 11, 2024, from https://capa-acam.ca/news/new-training-program-at-dalhousie-will-help-address-health-workforce-challenges
Cision PR Newswire. (2021, October 15). Physician Assistants Act in Nova Scotia Important Step in Health Modernization. Retrieved June 11, 2024, from https://www.newswire.ca/news-releases/physician-assistants-act-in-nova-scotia-important-step-in-health-modernization-847551751.html
Nova Scotia Health Authority. (2023, August 3). New Master’s Program to Train Physician Assistants. Retrieved June 11, 2024, from https://physicians.nshealth.ca/news/new-masters-program-train-physician-assistants
-
In October 2022, Newfoundland and Labrador’s Minister of Health announced plans to integrate Physician Assistants (PAs) into the province’s healthcare system. A year later, in November 2023, a three-year pilot program was launched, placing PAs across all five health zones.
PAs were introduced into a range of clinical settings, including inpatient care, surgery, hospitalist coverage, emergency departments, primary care, and follow-up for orphaned patients.
The pilot aims to strengthen healthcare delivery—particularly in rural and underserved areas—by increasing access to in-person care, reducing reliance on virtual services, and expanding preventive health efforts such as cancer screening.
References:
Government of Newfoundland and Labrador. (2019, July 29). New Public Health Legislation Now Law in Newfoundland and Labrador. Retrieved June 11, 2024, from https://www.gov.nl.ca/releases/2019/health/0729n02/
Canadian Association of Physician Assistants. (2023, November 6). 10 PAs coming to Newfoundland and Labrador to aid overworked doctors. Retrieved June 11, 2024, from https://capa-acam.ca/advocacy/press-releases/atlantic-provinces-call-on-physician-assistants-to-help-with-health-workforce-challenges-2023-04-05
Canadian Association of Physician Assistants. (2023, April 5). Atlantic Provinces Call on Physician Assistants to Help with Health Workforce Challenges. Retrieved June 11, 2024, from https://capa-acam.ca/advocacy/press-releases/atlantic-provinces-call-on-physician-assistants-to-help-with-health-workforce-challenges-2023-04-05
-
The inclusion of PAs in New Brunswick's healthcare system began in 2009 when the College of Physicians and Surgeons of New Brunswick (CPSNB) amended the New Brunswick Medical Act to include PAs. This legislation allowed for the licensing of PAs, enabling them to practice under the supervision of physicians and contribute significantly to the province's healthcare services.
New Brunswick has been proactive in integrating PAs into its healthcare teams, particularly through pilot programs aimed at demonstrating their value. One of the most notable pilot projects took place at Dr. Everett Chalmers Regional Hospital in Fredericton, where PAs were introduced to assist with surgical services. The success of this program led to its permanent establishment, showcasing the crucial role PAs play in improving patient care and reducing wait times.
There are ongoing discussions to introduce PAs into primary care and additional hospital settings.
References:
Canadian Association of Physician Assistants. (2024, October 18). Update from 2024 CAPA Annual Members Meeting. Ottawa, ON.
MacKay, F & Dickson, K. (2024, April 25). CAPA Webinar: Emergency Medicine Dr. Everett Chalmers Regional Hospital, Fredericton, NB [Webinar] https://capa-acam.ca/events/enhancing-healthcare-exploring-the-role-of-physician-assistants-april-25th-2024-04-25
Canadian Association of Physician Assistants. (2023, April 5). Atlantic Provinces Call on Physician Assistants to Help with Health Workforce Challenges. Retrieved June 11, 2024, from https://capa-acam.ca/advocacy/press-releases/atlantic-provinces-call-on-physician-assistants-to-help-with-health-workforce-challenges-2023-04-05
Canadian Association of Physician Assistants. (n.d.). PA Facts. Retrieved June 11, 2024, from https://capa-acam.ca/pa-facts
Canadian Association of Physician Assistants. (2023, November 6). 10 PAs coming to Newfoundland and Labrador to aid overworked doctors. Retrieved June 11, 2024, from https://capa-acam.ca/advocacy/press-releases/atlantic-provinces-call-on-physician-assistants-to-help-with-health-workforce-challenges-2023-04-05
-
In 2006, the Ontario Ministry of Health and Long-Term Care announced plans to introduce Physician Assistants (PAs) into the province. This led to the launch of the Ontario PA Demonstration Project in 2007, which placed PAs in various clinical settings to evaluate their impact on patient care and system efficiency. The success of this project laid the foundation for long-term integration and regulation.
On April 27, 2021, Ontario’s Minister of Health introduced legislation to formally regulate the PA profession. Bill 283, the Advancing Oversight and Planning in Ontario’s Health System Act, received Royal Assent on June 3, 2021. As of April 1, 2025, PAs in Ontario are regulated by the College of Physicians and Surgeons of Ontario (CPSO). This regulation ensures title protection, requires delegation by supervising physicians for controlled acts, and upholds consistent standards of care and professional accountability.
Ontario now joins provinces like Manitoba, New Brunswick, and Alberta in regulating PAs under their respective medical regulatory bodies.
The province is also home to two leading PA education programs: McMaster University’s PA Education Program, established in 2008, and the University of Toronto’s PA Professional Degree Program, launched in 2010. Both programs prepare students with the clinical and academic training needed to practice effectively in a variety of healthcare settings across Ontario.
References:
Canadian Association of Physician Assistants. (2021). Regulation of PAs in Ontario: Important step in health modernization. Retrieved April 25, 2024, from https://capa-acam.ca/2021/04/regulation-of-pas-in-ontario-important-step-in-health-modernization/
College of Physicians and Surgeons of Ontario. (2024). Physician assistants. Retrieved from https://www.cpso.on.ca/en/Physician-Assistants
Elliott, C. [@celliottability]. (2021, June 3). Excited to announce that Ontario is moving forward with regulating physician assistants [Tweet]. Twitter. https://twitter.com/celliottability/status/1400571891820253184
College of Physicians and Surgeons of Ontario. (2021, June 28). CPSO to regulate physician assistants. Retrieved April 25, 2024, from https://dialogue.cpso.on.ca/2021/06/cpso-to-regulate-physician-assistants/
HealthForceOntario. (n.d.). Physician Assistants. Retrieved June 11, 2024, from https://www.healthforceontario.ca/en/Home/Health_Providers/Physician_Assistants
-
In June 2023, the Government of Prince Edward Island (PEI), the College of Physicians and Surgeons of PEI, and Health PEI announced new regulations under the Regulated Health Professions Act that officially allow Physician Assistants (PAs) to practice in the province. This move is part of a broader strategy to strengthen the healthcare workforce and improve access to care.
The new regulations create a distinct registration class for PAs, enabling them to perform a range of medical duties under the supervision of licensed physicians.
PEI has since begun actively recruiting PAs to join Health PEI, with plans to hire five PAs to work in areas such as primary care, emergency medicine, and surgery. As of October 2024, the first PA is expected to begin practicing in the province, supported by a finalized regulatory framework.
References:
Canadian Association of Physician Assistants. (2024, October 18). Update from 2024 CAPA Annual Members Meeting. Ottawa, ON.
Government of Prince Edward Island. (n.d.). Associate physicians and physician assistants added to health care system. Retrieved April 25, 2024, from https://www.princeedwardisland.ca/en/news/associate-physicians-and-physician-assistants-added-to-health-care-system
Health PEI. (2023, November 3). Moving forward toward welcoming physician assistants. Retrieved April 25, 2024, from https://src.healthpei.ca/note-michael-nov-3-2023-moving-forward-toward-welcoming-physician-assistants
Government of Prince Edward Island. (n.d.). Hiring information for physician assistants. Retrieved April 25, 2024, from https://www.princeedwardisland.ca/en/information/health-and-wellness/hiring-information-for-physician-assistants
Government of Prince Edward Island. (2023, June 16). Physician Assistants Regulations. Retrieved June 11, 2024, from https://www.princeedwardisland.ca/en/information/health-and-wellness/physician-assistants-regulations
Government of Prince Edward Island. (2023, November 3). Province recruiting physician assistants to join health care system. Retrieved June 11, 2024, from https://www.princeedwardisland.ca/en/news/province-recruiting-physician-assistants-to-join-health-care-system
Government of Prince Edward Island. (2023, June 15). Associate Physicians and Physician Assistants added to health care system. Retrieved June 11, 2024, from https://www.princeedwardisland.ca/en/news/associate-physicians-and-physician-assistants-added-to-health-care-system
Canadian Association of Physician Assistants. (n.d.). PA Facts. Retrieved June 11, 2024, from https://capa-acam.ca/pa-facts
-
A pilot PA program in Quebec is underway, with Laval University considering a PA program.
References
Canadian Association of Physician Assistants. (2024, October 18). Update from 2024 CAPA Annual Members Meeting. Ottawa, ON.
-
The Medical Professional Amendment Act, 2023 introduced legislative changes that allow Physician Assistants (PAs) to practice in Saskatchewan and be regulated under the College of Physicians and Surgeons of Saskatchewan. PAs began integrating into the provincial healthcare system in early 2023, with roles in primary care, long-term care, emergency departments, oncology, general internal medicine, and surgery.
To support local training, the University of Saskatchewan’s College of Medicine will launch a two-year Master of Physician Assistant program in Fall 2025, with 20 seats in its first cohort. The program is tailored to address the province’s healthcare needs, particularly in rural and remote communities, and is supported by the College of Physicians and Surgeons of Saskatchewan.
These efforts are part of Saskatchewan’s broader plan to strengthen its healthcare system through targeted investments in workforce recruitment, education, and retention.
References:
Legislative Assembly of Saskatchewan. (2023). Bill 129: An Act to License Physician Assistants. Retrieved April 25, 2024, from https://docs.legassembly.sk.ca/legdocs/Bills/29L3S/Bill29-129.pdf
Government of Saskatchewan. (2023, March 30). Saskatchewan introduces legislation to license physician assistants. Retrieved April 25, 2024, from https://www.saskatchewan.ca/government/news-and-media/2023/march/30/saskatchewan-introduces-legislation-to-license-physician-assistants
Government of Saskatchewan. (2023, October 31). Physician assistant training program to proceed. Retrieved April 25, 2024, from https://www.saskatchewan.ca/government/news-and-media/2023/october/31/physician-assistant-training-program-to-proceed
Government of Saskatchewan. (n.d.). Physician Assistants. Retrieved June 11, 2024, from https://www.saskatchewan.ca/residents/health/health-human-resources/physician-assistants
Saskatchewan Health Authority. (n.d.). Physician Assistant. Retrieved June 11, 2024, from https://www.healthcareersinsask.ca/pa/
Canadian Association of Physician Assistants. (2024, October 18). Update from 2024 CAPA Annual Members Meeting. Ottawa, ON.
-
Military Physician Assistants (PAs) serve across Canada—including in remote regions like the Arctic—and may also be posted overseas or aboard naval ships. The PA role has deep roots in the Canadian Armed Forces (CAF), where the title “Physician Assistant” was first introduced in 1984 to describe senior medical personnel.
In 2002, the CAF launched a redesigned, two-year PA education program, which received national accreditation in 2004. Since then, the CAF has partnered with civilian universities, sponsoring students to complete accredited Canadian PA programs. After graduation, these PAs receive additional military-specific training to prepare them for work in challenging, often remote environments, including military bases, ships, and international deployments.
In 2016, PAs in the CAF were granted officer status, further recognizing their advanced training and leadership within military healthcare teams.
References
Canadian Association of Physician Assistants. (n.d.). Physician assistants in Canada. Retrieved November 9, 2024, from https://capa-acam.ca/
Canadian Armed Forces. (n.d.). Physician assistant. Canadian Armed Forces. Retrieved November 9, 2024, from https://forces.ca/en/career/physician-assistant/
Government of Canada. (2016, March 31). Evaluation of the Canadian Association of Physician Assistants Contribution Program (CAPA). Retrieved November 9, 2024, from https://www.canada.ca/en/department-national-defence/corporate/reports-publications/audit-evaluation/evaluation-canadian-association-physician-assistants-contribution-program.html
Keller, J. (2024). Physician assistant. Post-Secondary BC. Retrieved November 9, 2024, from https://www.postsecondarybc.ca/knowledgebase/physician-assistant/
PA Consortium (n.d.). A brief history of Emerging PA profession in Canada. Retrieved November 9, 2024, from https://paconsortium.ca/sites/default/files/PA_Brief_%20History_Canada_0.p
Canadian PA Organizations
-
JCANPA
-
ORTHO PA
Last updated June 12, 2025.